The mental health landscape has undergone a dramatic transformation in 2025, with virtual reality emerging as a game-changing therapeutic tool. What once seemed like science fiction has become an evidence-based treatment option that’s helping millions of people overcome anxiety, depression, PTSD, and chronic pain.
This technological revolution isn’t just changing how we treat mental health conditions—it’s redefining what’s possible in therapeutic care.
The Science Behind VR Therapy
Virtual reality therapy works by leveraging neuroplasticity, our brain’s ability to form new neural connections and adapt throughout life. When patients engage with immersive VR environments, their brains respond as if the experiences were real, triggering the same emotional and physiological responses they would have in actual situations.
Recent clinical studies have shown remarkable results. A 2024 meta-analysis published in the Journal of Medical Internet Research found that VR therapy achieved a 68% success rate in treating specific phobias, compared to 42% for traditional exposure therapy alone.
The controlled, repeatable nature of VR environments allows therapists to gradually expose patients to anxiety-inducing situations while maintaining complete safety and control.
The key lies in the brain’s inability to distinguish between virtual and real experiences when they’re sufficiently immersive.
This phenomenon, known as presence, creates authentic emotional responses that can be therapeutically harnessed and gradually modified through repeated exposure.
Specific Therapeutic Applications
Virtual Reality Exposure Therapy (VRET)
VRET has become the gold standard for treating phobias and anxiety disorders in 2025. Patients with a fear of flying can experience realistic airplane simulations, complete with turbulence and takeoff sensations, all from the safety of a therapist’s office.
Those with social anxiety can practice public speaking in virtual auditoriums filled with responsive digital audiences.
The therapy works through systematic desensitization. Patients start with less threatening virtual scenarios and progressively work up to more challenging situations.
A patient with agoraphobia might begin in an empty virtual park, then gradually experience busier environments with more people and activity.
PTSD Treatment Through Immersive Experiences
For veterans and trauma survivors, VR provides a controlled way to process traumatic memories. Combat veterans can revisit battlefield scenarios in a safe environment, allowing them to process their experiences with a trained therapist present. This approach has shown 73% improvement rates in PTSD symptoms, according to 2025 Department of Veterans Affairs data.
The technology allows for precise control over triggering elements. Therapists can adjust lighting, sounds, and environmental factors to match the patient’s comfort level and therapeutic needs.
This granular control makes it possible to work through trauma at the patient’s pace.
Mindfulness and Meditation in Virtual Worlds
VR meditation has evolved far beyond simple relaxation apps. Today’s platforms create immersive environments that respond to biometric feedback, adjusting visuals and sounds based on heart rate, breathing patterns, and stress indicators.
Patients might find themselves in a serene forest where the trees sway in rhythm with their breathing, or on a peaceful beach where waves match their heart rate.
These guided VR relaxation sessions have proven particularly effective in reducing stress. User’s report achieving meditative states 40% faster in VR compared to traditional meditation techniques.
The immersive nature eliminates external distractions that often derail conventional mindfulness practices.
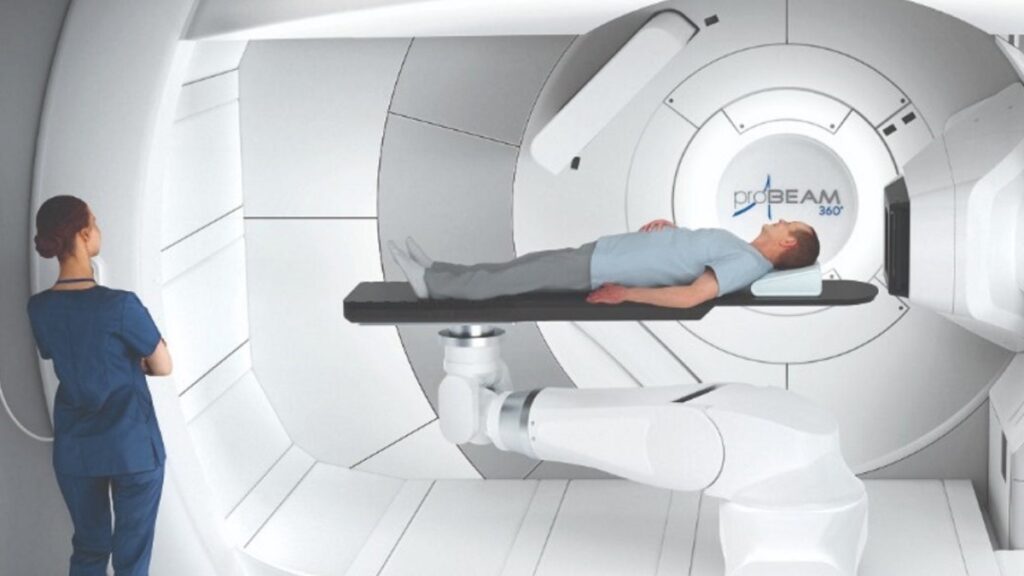
Pain Management Through Distraction Therapy
Virtual reality has revolutionized pain management, particularly for individuals with chronic conditions and those undergoing medical procedures. Burn patients undergoing wound care report 35-50% less pain when using VR distraction therapy. The technology works by overwhelming the brain’s pain-processing centers with immersive sensory input.
Patients might explore underwater worlds, play interactive games, or participate in guided breathing exercises while receiving medical treatment. The key is creating experiences engaging enough to redirect neural resources away from pain-processing pathways.
The Technology Behind the Therapy
Advanced VR Hardware
Modern therapeutic VR systems have evolved far beyond consumer gaming headsets. Medical-grade VR devices now feature:
- Ultra-high-resolution displays (8K per eye) that eliminate the “screen door effect” that once caused nausea
- Precise head tracking with sub-millimeter accuracy for natural movement
- Wireless connectivity that eliminates cables and improves safety
- Extended battery life supporting 4–6-hour therapy sessions
- Antimicrobial materials for safe use in medical environments
Biofeedback Integration
The most significant advancement in 2025 is the seamless integration of biofeedback devices with VR systems. Real-time monitoring of heart rate variability, skin conductance, breathing patterns, and even EEG brainwaves allows the virtual environment to respond to the patient’s physiological state.
When a patient’s stress levels spike during exposure therapy, the system can automatically adjust the intensity of the experience.
If someone practicing meditation shows signs of deep relaxation, the environment can enhance those conditions to deepen the therapeutic effect.

Haptic Feedback Systems
Advanced haptic technology now provides realistic touch sensations that enhance therapeutic presence. Patients can feel virtual textures, temperatures, and even simulated medical procedures. This tactile feedback is crucial for exposure therapy, making virtual experiences feel genuinely real.
AI-Powered Personalization
Artificial intelligence has transformed VR therapy from a one-size-fits-all approach to highly personalized treatment plans. Machine learning algorithms analyze patient responses, treatment progress, and biometric data to create customized therapeutic experiences.
The AI continuously adapts scenarios based on patient needs. If someone with social anxiety shows progress in one-on-one virtual conversations, the system gradually introduces group settings.
For PTSD patients, AI can identify specific triggers and create targeted exposure scenarios while avoiding elements that might cause harmful re-traumatization.
Predictive analytics enable therapists to identify potential treatment roadblocks before they arise. The system can flag patterns that suggest a patient might discontinue treatment, allowing therapists to intervene with modified approaches or additional support.
Benefits of Transforming Mental Health Care
Unprecedented Accessibility
VR therapy has dramatically improved access to mental health treatment. Patients in remote areas can now access specialized therapy without traveling hundreds of miles. The technology has enabled the delivery of world-class treatment to underserved communities through telemedicine platforms.
For patients with mobility issues, severe agoraphobia, or other conditions that make leaving home challenging, VR therapy provides treatment options that were previously impossible.
Home-based VR therapy systems, supervised remotely by licensed therapists, have opened treatment doors for thousands of patients.
Enhanced Patient Engagement
Traditional therapy often struggles with patient adherence to treatment plans. VR therapy has achieved engagement rates of 89%, compared to 64% for traditional therapy methods. The immersive, interactive nature of VR makes therapy sessions feel less like medical appointments and more like engaging experiences.
Patient’s report looking forward to VR therapy sessions. The technology gamifies treatment progress, providing immediate feedback and measurable improvements that motivate continued participation.
Visual progress tracking through virtual environments gives patients tangible evidence of their improvement.
Consistent Treatment Quality
VR standardizes therapeutic experiences in ways traditional therapy cannot. Every patient receives the same high-quality exposure scenario, eliminating variability that can occur with role-playing or imagination-based techniques. This consistency improves treatment outcomes and makes it easier to measure therapeutic effectiveness.
Therapists can replicate successful treatment protocols exactly, sharing effective VR scenarios with colleagues worldwide. This standardization has accelerated the development and validation of new therapeutic approaches.
Addressing the Challenges
Data Privacy and Security
The immersive nature of VR therapy generates unprecedented amounts of personal data. Biometric information, behavioral patterns, emotional responses, and treatment progress create detailed psychological profiles that require robust protection.
Leading VR therapy platforms in 2025 utilize end-to-end encryption, blockchain-based consent management, and federated learning techniques, which keep sensitive data on local devices.
Regulatory frameworks, such as the updated HIPAA guidelines for digital therapeutics, provide clear standards for data handling and patient privacy.
However, concerns persist about data breaches and the potential misuse of sensitive psychological information. The industry continues to work on balancing therapeutic effectiveness with privacy protection.
Ethical Considerations in Immersive Treatment
VR therapy raises unique ethical questions. The technology’s ability to create intensely realistic experiences means therapists must carefully consider the potential for re-traumatization or unintended psychological effects. Professional guidelines now require specialized training in VR ethics for practitioners.
Questions about informed consent become complex when dealing with immersive experiences that feel real. Patients must understand not just the therapeutic goals but also the potential psychological impact of virtual experiences.
Clear protocols now exist for obtaining appropriate consent and providing adequate preparation for VR therapy.
Technology Barriers and Costs
Despite decreasing prices, high-quality therapeutic VR systems remain expensive. A complete setup costs between $15,000 and $50,000, which limits adoption in smaller practices and community mental health centers. However, insurance coverage is expanding, with major providers now covering VR therapy for specific conditions.
Technical support and maintenance require specialized knowledge that many healthcare facilities lack. The industry has responded by developing cloud-based platforms that reduce local technical requirements and provide ongoing support services.
Training and Professional Development
The rapid adoption of VR therapy has created an urgent need for specialized training programs. Medical schools and psychology programs are now incorporating VR therapy courses into their curricula. Professional certification programs have emerged to ensure that therapists understand both the therapeutic applications and technical aspects of VR systems.
Training programs focus on:
- Technical proficiency with VR hardware and software
- Therapeutic protocol development for virtual environments
- Biometric data interpretation and treatment adjustment
- Ethical considerations specific to immersive therapy
- Emergency procedures for VR-induced adverse reactions
Continuing education requirements now include VR therapy components, ensuring practitioners stay current with rapidly evolving technology and techniques.
Future of Digital Well-being
As we look toward the future, VR therapy represents just the beginning of a broader digital well-being revolution. Emerging technologies promise even more sophisticated therapeutic possibilities.
Integration with Daily Life
Future VR systems will seamlessly integrate with daily routines. Patients might receive micro-interventions throughout the day—brief VR sessions triggered by stress indicators from wearable devices. Smart environments could automatically adjust lighting, sound, and even scent to support therapeutic goals.
Advanced Biometric Integration
Next-generation systems will incorporate real-time brain imaging, allowing therapists to observe neural activity during treatment. This neurofeedback will enable unprecedented precision in therapeutic interventions, potentially reducing treatment times and improving outcomes.
Collective Virtual Therapy
Group therapy is evolving toward shared virtual spaces where patients can interact with others facing similar challenges. These virtual support communities provide peer support and social connection while maintaining privacy and safety.
Measuring Success and Outcomes
The quantifiable nature of VR therapy has revolutionized outcome measurement in mental health treatment. Traditional therapy relies heavily on subjective reports and standardized questionnaires. VR therapy provides objective data through:
- Physiological responses during exposure scenarios
- Behavioral patterns within virtual environments
- Treatment adherence through automatic session tracking
- Progress visualization through comparative virtual assessments
This data-driven approach has enabled more precise treatment adjustments and improved therapeutic outcomes. Insurance providers are increasingly favoring VR therapy due to its measurable results and evidence-based effectiveness.
To Conclude
Virtual reality has fundamentally transformed mental health therapy in 2025, offering hope to millions who previously struggled with limited treatment options. The technology’s ability to create safe, controlled, and immersive therapeutic experiences has opened new possibilities for treating anxiety, depression, PTSD, and chronic pain.
The integration of AI, biofeedback, and advanced haptic systems has created personalized treatment experiences that adapt to individual patient needs. While challenges around privacy, ethics, and accessibility remain, the mental health field continues to develop solutions that prioritize patient welfare and therapeutic effectiveness.
The future of digital well-being looks brighter than ever, with VR leading the charge toward a world where quality mental health treatment is available to anyone, anywhere, at any time.

